Introduction
Celiac disease diagnosis often feels like a long, painful mystery rather than a straightforward test result. As a physician, I’ve seen countless patients who have suffered for years with vague digestive issues bloating, fatigue, anemia only to discover later that gluten has been silently damaging their intestines.
Many people go undiagnosed or misdiagnosed for years because celiac disease can mimic so many other conditions. Understanding how to identify it early can prevent long term complications like nutrient deficiencies, osteoporosis, infertility, and even certain cancers.
Let’s uncover the truth about celiac disease diagnosis, the challenges behind it, and how modern medicine is improving accuracy and speed.
What is the celiac disease diagnosis process?
Diagnosis of celiac disease involves a combination of blood tests and an intestinal biopsy to confirm the body’s immune response to gluten.
The first step is usually a serologic test, which measures specific antibodies such as tissue transglutaminase (tTG-IgA) and endomysial antibodies (EMA). If these antibodies are elevated, it suggests that gluten is triggering an immune response.
The doctor then performs an upper endoscopy to collect small samples from the small intestine. A pathologist examines them under a microscope to detect villi damage, which confirms the diagnosis.
It is important not to start a gluten free diet before testing because this can falsely normalize the results.
Diagnosis of celiac disease also includes ruling out other conditions such as irritable bowel syndrome (IBS) or lactose intolerance.
(Source: CDC, Mayo Clinic)

Understanding the Basics of Celiac Disease Diagnosis
Diagnosing of celiac disease isn’t as simple as a blood test. It’s a multi step process that combines medical history, antibody tests, genetic screening, and an intestinal biopsy to confirm the disease.
The reason? Celiac disease is a complex autoimmune disorder, not just a food intolerance. When gluten (a protein found in wheat, barley, and rye) is eaten, it triggers the immune system to attack the lining of the small intestine.
Over time, this damages the villi, the tiny finger like structures that absorb nutrients. As the villi flatten, nutrient absorption decreases leading to anemia, weight loss, fatigue, and even neurological symptoms.
The hidden challenge ( why celiac disease is often underdiagnosed).
Globally, it is estimated that up to 80% of people with celiac disease are undiagnosed. Many live for years with symptoms attributed to stress, IBS, or food allergies.
Why? Because symptoms are highly variable. Some patients experience severe diarrhea and weight loss. Others experience only fatigue, headaches, or joint pain.
As a physician, I once had a patient who came in for chronic anemia. He had no digestive symptoms, yet his biopsy later revealed celiac disease.
This variability makes diagnosing celiac disease difficult and necessary. Without it, ongoing inflammation silently damages the intestines, increasing the risks of osteoporosis, infertility, and intestinal lymphoma.
Step-by-step process for diagnosing celiac disease
1. Clinical evaluation and medical history
The journey begins with a detailed clinical evaluation. Your doctor will ask about:
- Digestive symptoms (diarrhea, bloating, abdominal pain)
- Non digestive symptoms (fatigue, anemia, joint pain, infertility)
- Family history of celiac or autoimmune diseases
- Previous dietary changes or gluten-free efforts.
If celiac disease is suspected, blood tests are ordered.
2. Serologic (blood) tests
The cornerstone of celiac disease diagnosis is the tissue transglutaminase IgA (tTG-IgA) test. It detects antibodies that your immune system makes against gluten induced inflammation.
Other useful blood tests include:
- Endomysial antibody (EMA): Highly specific for celiac disease.
- Deamidated gliadin peptide (DGP): Useful when tTG results are unclear.
- Total IgA: Helps detect IgA deficiency, which can cause false negatives.
Important note:
Do not start a gluten-free diet before these tests, This can normalize antibody levels and lead to a false negative result.
(Source: PubMed, 2024 Review on Serologic Accuracy in Celiac Diagnosis)
3. Genetic Testing (HLA Typing)
- Celiac disease has a strong genetic link. Approximately 95% of patients carry the HLA-DQ2 gene, and most of the remaining 5% carry HLA-DQ8.
- A negative HLA-DQ2/DQ8 test can rule out celiac disease in most cases. However, having these genes does not confirm the disease, They only indicate susceptibility.
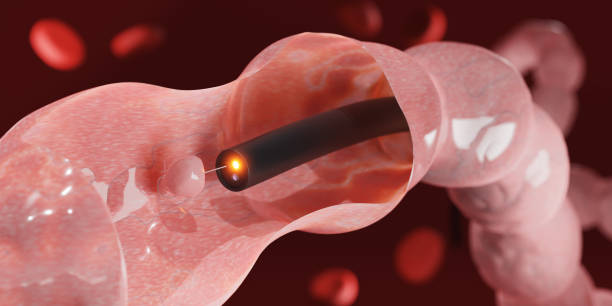
4. Endoscopy and small bowel biopsy
This is the gold standard for confirming a diagnosis of celiac disease.
- During an upper endoscopy, the doctor inserts a thin, flexible tube with a camera through the mouth into the small intestine. Small tissue samples (biopsies) are collected for microscopic examination.
- If the villi appear blunt or flattened, this confirms the diagnosis. The degree of villous atrophy is graded using the Marsh grading system.
For patients who have already started a gluten-free diet, a gluten challenge (temporarily reintroducing gluten before testing) may be required for accurate results.
5. Diagnosis of celiac disease in children
In children, the diagnosis can sometimes be made without biopsy if antibody levels are very high and symptoms are typical. This approach follows the guidelines of the European Society for Pediatric Gastroenterology (ESPGHAN).
However, US recommendations (Mayo Clinic) still prefer biopsy confirmation in most cases to avoid misdiagnosis.
Conditions that mimic celiac disease.
Misdiagnosis is one of the greatest challenges. Celiac disease symptoms overlap with several gut disorders, including:
- Irritable bowel syndrome (IBS)
- Lactose intolerance
- Crohn’s disease
- Non celiac gluten sensitivity
- Small intestinal bacterial overgrowth (SIBO)
That’s why proper testing under medical supervision is so important before making dietary changes.
Read in Detail About:[ Irritable Bowel Syndrome Diagnosis ]
[Irritable Bowel Syndrome Symptoms]
What happens after a diagnosis?
Once confirmed, treatment focuses on complete gluten avoidance. A gluten-free diet allows the gut to heal and antibodies to normalize.
Follow-up testing
- Repeat antibody testing after 6-12 months
- Check for nutritional deficiencies (iron, folate, vitamin D, B12)
- Bone density scan (especially in adults)
- Assessment of hidden gluten exposure
- Even small traces of gluten can trigger inflammation. Ongoing follow-up ensures true recovery and prevents complications.
Read more: [Foods to Avoid in Celiac Disease] [Foods Good for Celiac Disease]
A Doctor’s Unique Insight ( The Hidden Side of Celiac Disease).
Many blogs miss this important medical insight: Celiac disease does not always go away with dietary management.
Up to 10% of patients have refractory celiac disease, where the gut does not heal even after strict gluten elimination. This condition may require steroid or immunosuppressive therapy under specialist care.
As a physician, I always emphasize:
“Celiac disease is not just a gut problem, it’s an immune condition that requires lifelong vigilance.”
That’s why early and accurate diagnosis is crucial, it prevents chronic inflammation from escalating into serious complications.
Patient Story (Missed Diagnosis)
Emma, a 35 year old graphic designer, came to my clinic complaining of fatigue and brittle nails. She had been told for years that she was “just anemic.”
A simple tTG-IgA test later revealed sky high antibody levels. A biopsy confirmed celiac disease. After six months on a strict gluten-free diet, her iron levels returned to normal, and her energy returned.
Emma’s story illustrates a painful truth: the diagnosis of celiac disease often comes late after years of silent loss.
Complications of Delayed Diagnosis of Celiac Disease
When left undiagnosed, celiac disease can cause serious long-term harm, including:
- Osteoporosis (due to calcium and vitamin D malabsorption)
- Infertility and miscarriage
- Nerve problems (peripheral neuropathy, brain fog)
- Increased risk of intestinal lymphoma.
Early diagnosis is not just about symptom relief it’s about protecting long term health.
Practical tips for patients awaiting celiac disease diagnosis
While waiting for test or biopsy results, follow these practical steps:
- Do not start a gluten-free diet until the test is complete.
- Keep a symptom diary, Note food triggers, fatigue, and bowel changes.
- Ensure a balanced diet rich in fruits, vegetables, and lean protein.
- Manage stress, This can worsen bowel symptoms.
Ask your doctor about testing for related conditions like thyroid disease or type 1 diabetes.
Read More: [Gluten Free Foods] [Foods that relieve gas and bloating]

Bottom Line (A celiac disease diagnosis saves lives).
An accurate diagnosis of celiac disease changes everything. It’s the difference between silent suffering and active healing.
With modern testing from antibodies to biopsies detection is more accurate than ever. Early diagnosis prevents irreversible intestinal damage and restores quality of life.
Remember: Don’t self diagnose or rely solely on “gluten-free trends.” Always consult a medical professional for accurate diagnosis and management.
Call to Action
If you’re struggling with unexplained gut issues, fatigue, or nutritional deficiencies, don’t ignore the symptoms.
Schedule your celiac disease diagnosis today early testing means faster healing and a healthier future.
Have questions or personal experiences to share? Comment below or consult with me directly together, we will uncover the truth behind your symptoms and guide you towards recovery.
References:
FAQS
Yes. It can appear at any age, even in people who previously tolerated gluten. Environmental triggers and gut infections can activate genetic susceptibility.
In children with very high antibody levels, yes but most adults still require biopsy for confirmation.
It involves antibody blood tests (tTG-IgA, EMA) followed by a small intestine biopsy to confirm villi damage. Genetic testing may also support the diagnosis.
No. You must continue eating gluten before testing, or your antibody levels may normalize, giving a false-negative result.
You may have non-celiac gluten sensitivity. Your doctor can help differentiate this condition through elimination diets and specialized tests.
🧑⚕️ About the Author
Dr. Asif, MBBS, MHPE
Dr. Asif is a licensed medical doctor and qualified medical educationist with a Master’s in Health Professions Education (MHPE) and 18 years of clinical experience. He specializes in gut health and mental wellness. Through his blogs, Dr. Asif shares evidence-based insights to empower readers with practical, trustworthy health information for a better, healthier life.
⚠️ Medical Disclaimer
This blog is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard or delay medical advice based on content you read here.


Leave a Reply