Introduction
Causes of hypothyroidism in females is important to understand, because hypothyroidism, or an underactive thyroid, occurs when the thyroid gland does not produce enough hormones to meet the body’s needs. These hormones regulate metabolism, energy production, and overall bodily functions. Although hypothyroidism can affect anyone, it is more common in women. Recognizing the causes of hypothyroidism in women is essential for early detection, prevention, and effective management.
What you will learn in this blog:
- Major causes of hypothyroidism in women – autoimmune, genetic, and hormonal factors
- Risks specific to women – Why women are more susceptible than men.
- Environmental and lifestyle contributors – Diet, stress, chemicals, and sleep
- Medical and surgical triggers – Medications, thyroid surgery, and radiation
- Early detection and prevention tips – How to protect your thyroid health
What are the causes of hypothyroidism in females?
Hypothyroidism in women can be caused by a variety of factors, including autoimmune diseases such as Hashimoto’s thyroiditis, iodine deficiency, certain medications, and previous thyroid surgery. Women are more susceptible to these causes due to hormonal fluctuations, genetic predisposition, and differences in the immune system. Recognizing these causes is crucial for timely diagnosis and treatment.
1. Thyroiditis: Inflammation that can silence your thyroid.
Thyroiditis refers to inflammation of the thyroid gland, which can temporarily or permanently reduce hormone production. Thyroiditis is one of the main causes of hypothyroidism in females.
- Hashimoto’s thyroiditis is the most common form in women, where the immune system gradually attacks thyroid tissue.
- Subacute thyroiditis can occur after a viral infection, causing initial hyperthyroidism followed by hypothyroidism.
Symptoms include fatigue, mild neck swelling, and sensitivity to cold.

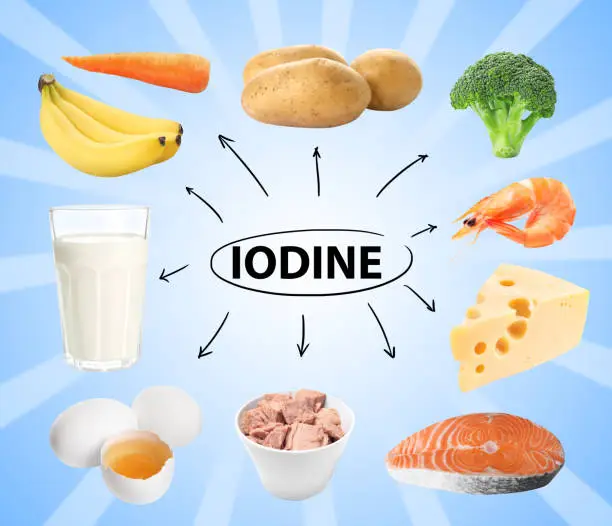
2. Iodine deficiency: a preventable cause
Iodine is essential for the production of thyroid hormones. Insufficient iodine deficiency can lead to hypothyroidism, especially in areas where iodine deficiency is high. Although iodine deficiency has become less common in many parts of the world due to iodized salt programs, it remains a significant problem in some areas.
Read Here Iodine Rich foods in Detail
3. Medications and Treatments
Some medications and medical treatments can interfere with thyroid function, resulting in hypothyroidism. Women taking these treatments should be aware of the risks and monitor their thyroid health regularly.
Common medications and treatments associated with hypothyroidism include:
- Radioactive iodine therapy: Often used to treat hyperthyroidism or thyroid cancer, this therapy can destroy thyroid tissue, sometimes leading to permanent hypothyroidism.
- Antithyroid medications: Medications such as methimazole or propylthiouracil, which are used to control hyperthyroidism, can reduce thyroid hormone production too much in some patients.
- Lithium: A medication commonly prescribed for bipolar disorder, lithium can impair thyroid hormone synthesis and increase the risk of hypothyroidism.
- Amiodarone: This heart medication contains iodine and can affect thyroid function, causing hypo or hyperthyroidism.
- Interferon therapy: Used for certain viral infections and cancers, interferon can trigger autoimmune thyroiditis.
- Tyrosine Kinase Inhibitors (TKIs): Some cancer treatments in this category have been associated with thyroid dysfunction.
Clinical insight: In my experience, patients on long term lithium or amiodarone therapy often need routine thyroid function tests to catch early signs of hypothyroidism before symptoms become severe.
4. Radiation Exposure
Radiation therapy to the neck or chest, commonly used to treat cancers, can damage thyroid tissue and reduce hormone production, leading to hypothyroidism. Even low dose exposure from medical imaging or environmental sources may slightly increase risk over time.
Clinical Tip: Women who have received neck or chest radiation should have regular thyroid function tests to detect any changes early.
5. Thyroid surgery: When treatment becomes a cause.
- Surgical removal of all or part of the thyroid, often done for lumps, nodules, or cancer, can result in hypothyroidism.
- The extent of the surgery determines the risk: A total thyroidectomy almost always requires lifelong hormone replacement.
- Even partial removal can reduce hormone production in some women.
- Post surgery monitoring is necessary to properly adjust thyroid hormone doses.
6. Congenital hypothyroidism: Present from birth
- Some women are born with an underactive thyroid due to developmental defects or genetic conditions.
- Newborns are usually screened at birth for early detection.
- Untreated congenital hypothyroidism can lead to developmental delays, growth problems, and cognitive impairment.
- Early diagnosis and hormone replacement therapy can prevent long term complications.
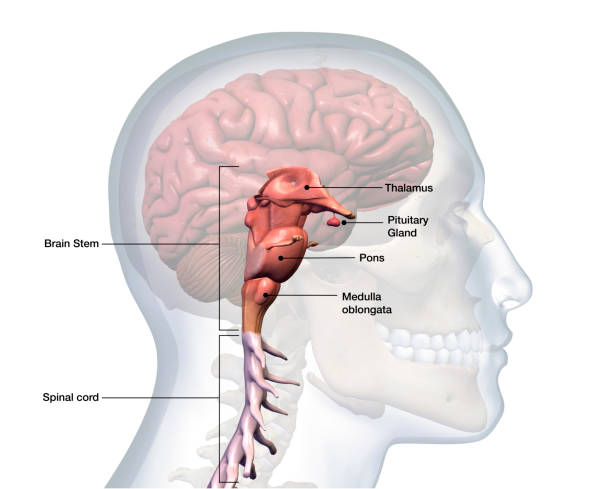
7. Pituitary gland dysfunction: When the “master gland” fails.
- The pituitary gland produces thyroid stimulating hormone (TSH), which tells the thyroid how much hormone to secrete.
- Pituitary disorders, such as tumors or pituitary insufficiency, can cause secondary hypothyroidism.
- Unlike primary hypothyroidism, the problem originates in the pituitary, not the thyroid.
- Symptoms are similar but can occur with other hormone deficiencies, including adrenal or reproductive hormones.
8. Environmental and Lifestyle Factors: Modifiable Contributors
Environmental Exposures
Several environmental factors can influence thyroid health:
Iodine Intake: Both deficiency and excess iodine can lead to thyroid dysfunction. Wikipedia
Chemical Exposures: Endocrine disrupting chemicals like bisphenols and phthalates can interfere with thyroid hormone synthesis and action. Frontiers
Radiation Exposure: Exposure to radiation, whether from medical treatments or environmental sources, increases the risk of thyroid disorders. PMC
Lifestyle Factors
Modifiable lifestyle choices can impact thyroid function:
Dietary Habits: A diet lacking in essential nutrients like selenium, vitamin D, and iodine can impair thyroid health. READ IN DETAIL ABOUT:BEST MULTIVITAMINS AND MINERALS FOR HYPOTHYROIDISM
Physical Activity: Regular exercise supports overall health and can help maintain optimal thyroid function.
Stress Management: Chronic stress can lead to hormonal imbalances that affect thyroid health.
Sleep Patterns: Adequate sleep is crucial for hormonal regulation and thyroid health.
Read here in details about:Thyroid-friendly foods for hypothyroidism
9. Other Medical Conditions
Some medical conditions can increase the risk of hypothyroidism by affecting immune function, thyroid tissue, or hormone regulation. Women should be especially careful in these situations.
Medical conditions closely associated with hypothyroidism include:
- Type 1 diabetes: Autoimmune diabetes increases susceptibility to autoimmune thyroid diseases.
- Down syndrome: Genetic predisposition increases the risk of congenital and acquired hypothyroidism.
- Turner syndrome: A chromosomal disorder in women that often affects thyroid function.
- Addison’s disease: Autoimmune adrenal insufficiency can occur with autoimmune thyroid disease.
- Celiac disease: Gluten intolerance and autoimmune gut problems can be linked to thyroid autoimmunity.
- Rheumatoid arthritis and lupus: Other autoimmune disorders increase the risk of Hashimoto’s thyroiditis.
- Pernicious anemia: Spontaneous destruction of gastric parietal cells may be associated with thyroid autoimmunity.
Clinical insight: In my practice, women with multiple autoimmune conditions often exhibit subtle changes in thyroid function, highlighting the importance of regular monitoring even before overt hypothyroid symptoms appear.
10. Why are women at higher risk for thyroid disorders?
Thyroid disorders, especially hypothyroidism, are significantly more common in women than in men. This increased risk is influenced by age, hormonal fluctuations, and unique differences in the immune system. Understanding these factors helps in early detection, prevention, and better management of thyroid health.
1. Hormonal Influence: Estrogen and Thyroid Function
Estrogen and Thyroid Function: Estrogen can affect thyroid hormone levels by increasing the amount of thyroid binding globulin (TBG), a protein that carries thyroid hormones in the blood. High TBG can reduce the amount of free, active thyroid hormone, especially during pregnancy or hormone therapy.
Life Stage Vulnerability: Women may experience thyroid imbalances due to rapid hormonal changes during puberty, pregnancy, postpartum, and menopause.
Clinical Insight: In my experience, women with fluctuating estrogen levels often report fatigue, mood swings, and weight gain that can be mistakenly attributed to aging or lifestyle rather than thyroid dysfunction.
2. Age related risk factors
Middle age and beyond: Women over 40-50 years of age, especially during perimenopause and menopause, show a higher prevalence of hypothyroidism.
Changes in the immune system: Aging can affect the activity of the immune system, making it more likely to develop autoimmune thyroid diseases such as Hashimoto’s.
Population data: Studies show that approximately 10% of women over 50 have subclinical or overt hypothyroidism (CDC, 2023).
3. Autoimmunity in women
- Women are more prone to autoimmune conditions, which directly contribute to thyroid dysfunction.
- Hormonal influences, especially estrogen, alter the immune response, sometimes triggering attacks on thyroid tissue.
This explains why autoimmune causes is the main causes of hypothyroidism in females, including Hashimoto’s thyroiditis and Subacute thyroiditis.
4. Pregnancy and postpartum risk
Postpartum thyroiditis: After delivery, some women experience temporary inflammation of the thyroid, leading to hypothyroidism or hyperthyroidism.
Long term implications: Even if temporary, postpartum thyroiditis can increase the risk of permanent hypothyroidism later in life.
Clinical tip: Routine thyroid function testing is recommended for women with symptoms such as fatigue or mood changes in the postpartum period.
5. Summary insights
Women’s unique hormonal environment, combined with age related immune changes and genetic predisposition, puts them at higher risk for thyroid disorders. Early awareness, routine screening in high risk groups, and lifestyle measures can significantly reduce the complications of hypothyroidism.
Conclusion
Causes of hypothyroidism in women can range from autoimmune diseases and iodine deficiency to medications, surgery, and hormonal changes. Understanding these triggers is essential for early detection, effective treatment, and long term thyroid health. Women, especially those with a family history of thyroid disorders or at certain stages of life such as pregnancy or menopause, should be vigilant.
By recognizing silent symptoms, making informed lifestyle choices, and promptly consulting a healthcare professional, you can effectively manage hypothyroidism and maintain overall health. Remember, early awareness and timely intervention make a significant difference in quality of life.
Call to Action:
If you notice symptoms like fatigue, unexplained weight gain, or mood swings, don’t wait consult your doctor, ask questions, and take proactive steps to protect your thyroid health. Share your experiences or concerns in the comments below to help others learn from your journey.
FAQS
Most primary hypothyroidism requires lifelong treatment. Early diagnosis and proper levothyroxine therapy can normalize hormone levels and prevent complications.
Yes. Lithium, amiodarone, immunotherapy, and radiation can reduce thyroid hormone production, leading to hypothyroidism.
The main causes include autoimmune disease (Hashimoto’s), iodine deficiency/excess, medications, congenital defects, thyroid surgery, and pituitary disorders. Women are disproportionately affected.
Congenital thyroid malformation, genetic enzyme defects, or maternal iodine deficiency can cause hypothyroidism in children. Early detection prevents growth and developmental delays.
Hormonal fluctuations, autoimmune susceptibility, and pregnancy-related changes increase hypothyroidism risk in women.
🧑⚕️ About the Author
Dr. Asif, MBBS, MHPE
Dr. Asif is a medical doctor and medical educationist with expertise in simplifying complex health topics for the general public. With a passion for preventive health and evidence-based writing, he helps readers make informed choices about their well-being.
✅ Medically Reviewed By
Dr. T.G., MBBS, FCPS (Endocrinology)
Associate Professor, Endocrinology Ward, HMC Hospital
With over 20 years of clinical experience in managing endocrine disorders, Dr. T.G. ensures that the content is accurate, reliable, and clinically relevant.
⚠️ Medical Disclaimer
This blog is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard or delay medical advice based on content you read here.

Leave a Reply