Introduction
Primary biliary cirrhosis treatment is one of the most common concerns my patients ask when they are newly diagnosed with this chronic liver condition. As a licensed physician and medical educator, I know how overwhelming it can feel to hear the word cirrhosis. Many people immediately think of irreversible damage or hopelessness, but the reality today is very different.
Modern medicine has provided us with effective primary biliary cirrhosis treatment and strategies that can slow the progression of the disease, reduce symptoms like fatigue and itching, and help patients live longer, healthier lives. This blog is designed to provide you with clear, reliable information the way I would explain it to a concerned patient in my clinic. Whether you are managing PBC yourself, helping a loved one, or simply learning, you will find practical insight, hope, and empowerment here.
What is the treatment of primary biliary cirrhosis?
Primary biliary cirrhosis treatment focuses on slowing liver damage, relieving symptoms, and preventing complications. While there is currently no cure, effective medications and lifestyle changes can help patients live longer, healthier lives.
The first line treatment of primary biliary cirrhosis is ursodeoxycholic acid (UDCA), which improves bile flow and slows disease progression. If UDCA alone is not effective, obeticholic acid (OCA) may be added. To relieve symptoms, doctors may recommend medications for itching, vitamin supplements for deficiencies, and monitoring of bone health. In advanced cases where the liver has been severely damaged, a liver transplant may be necessary and offers the best survival rate. Along with medications, patients are encouraged to follow a liver friendly diet, avoid alcohol, and manage fatigue. With proper treatment and monitoring, many people with PBC live full lives.
Understanding Primary Biliary Cirrhosis
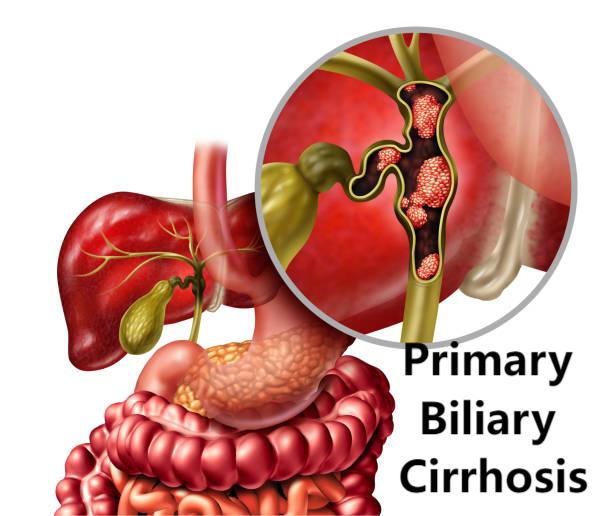
When we talk about primary biliary cirrhosis (PBC) now commonly called primary biliary cholangitis we’re describing a chronic autoimmune disease of the liver. Let’s break it down step by step so you can clearly understand what’s going on inside the body.
What happens in PBC?
- Your liver has tiny tubes called bile ducts that carry bile (a digestive fluid) from the liver to the intestine.
- In PBC, the immune system mistakenly attacks these tiny bile ducts, damaging them over time.
- As these ducts become scarred, bile can’t flow properly. It starts to build up in the liver, causing irritation and inflammation.
- This ongoing injury gradually leads to fibrosis (scarring) and eventually cirrhosis, which is an advanced stage of liver scarring.
Analogy: Think of your liver as a busy factory that produces bile. The bile ducts are like tiny pipelines. If workers accidentally start destroying these pipelines, waste builds up, machinery rusts, and the factory becomes less efficient.
Who gets PBC?
- PBC is more common in women (about 90% of cases), especially those aged 30-60.
- It is considered relatively rare, affecting about 1 in 1,000 women over the age of 40 in some populations (PubMed, 2020).
- While men can get PBC, it is much less common.
Why does it happen?
The exact cause is still unclear, but research suggests that it is due to a combination of factors:
- Genetic predisposition – if someone in your family has PBC or other autoimmune diseases, you are at higher risk.
- Autoimmunity – the body’s immune system mistakenly identifies the bile ducts as “foreign” and attacks them.
- Environmental triggers – infections, smoking, or certain toxins can trigger an immune response in susceptible people.
Overview of primary biliary cirrhosis treatment
The goal of primary biliary cirrhosis treatment is to:
- Slow the progression of the disease.
- Relieve symptoms such as itching, fatigue, or dry mouth.
- Prevent complications such as osteoporosis, cirrhosis, or liver failure.
- Maintain quality of life
Unlike in the old days when little could be done, there are several effective treatments today, which are improving both survival and quality of life.
First-line therapy
Ursodeoxycholic Acid (UDCA)
- Considered the gold standard treatment.
- Dosage: 13-15 mg/kg per day.
- Works by improving bile flow, reducing inflammation, and reducing fibrosis.
- Long term studies have shown that Ursodeoxycholic acid improves transplant free survival (PubMed, Lindor et al. 2019).
Doctor’s insight: Many patients are wary of lifelong medication, but Ursodeoxycholic acid is generally safe, well tolerated, and often an excellent long-term companion for managing PBC.
How long before it works?
- Most patients respond within 1 year.
- If liver tests (e.g. ALP, bilirubin) improve, the prognosis is excellent.
Second-line therapy
Obeticholic acid (OCA)
- Used when patients do not respond adequately to Ursodeoxycholic acid.
- Works by activating FXR receptors to reduce bile acid production.
- Improves lab markers and slows fibrosis.
Fibrates (bizofibrate, fenofibrate)
- Although not specifically FDA-approved for PBC, studies show that they reduce itching and improve liver enzymes.
- Useful in combination with UDCA.
Symptom management
Living with PBC is not just about lab tests it’s about quality of life. Many patients experience fatigue, itching, or bone pain.
Fatigue
- Very common and often frustrating.
- Management includes light exercise, sleep hygiene, and treatment of contributing factors such as thyroid disease.
Pruritus (itching)
- Due to bile acid buildup.
Treatment:
- Cholestyramine (first line)
- Rifampicin
- Naltrexone (in resistant cases)
Bone health
- Patients with PBC are at increased risk of osteoporosis.
Preventive measures:
- Calcium + Vitamin D
- Weight-bearing exercises.
- Bone density scan (DEXA)
Read in Detail About: [How to keep your liver healthy]
Latest treatment of primary biliary cirrhosis
Liver transplantation
- Reserved for end-stage disease or severe complications.
- The 5-year survival rate after transplant is >80% (Mayo Clinic data).
- Many patients return to normal life after transplant.

Novel Treatments of primary biliary cirrhosis which is Under Investigation
- Seladelpar (PPAR-delta agonist) shows promising results.
- Immune-modulating drugs are being tested to reduce autoimmune attacks.
Doctor’s Insight (Unique): One overlooked aspect is patient education. I have seen patients who have delayed care because they thought itchiness or fatigue was “just age.” Early detection can add years of healthy life.
Lifestyle and Self-Care
Dietary Tips
- A balanced diet with fresh fruits, vegetables, lean protein.
- Avoid excessive salt (especially if ascites occurs).
- Avoid alcohol completely.
Vaccination
- Hepatitis A and B vaccines are recommended if not already immune.
Read in Detail About: [hepatitis B vaccine adult schedule]
Surveillance
- Regular liver function tests.
- Screening for cirrhosis and portal hypertension.
Read in Detail About: [Cirrhosis Self-Care]
Prognosis and Life Expectancy
With modern treatments such as UDCA and OCA, life expectancy has improved significantly. Many patients live normal or near normal lives, especially if diagnosed early.
According to a WHO review (2020), the 10 year transplant-free survival rate of responders to UDCA is over 90%.
Prognosis depends on the stage of diagnosis, response to treatment, and lifestyle.
Read in Detail: [Liver Life Expectancy Stage 4 Cirrhosis]
Coping with Emotional Impact
- Chronic illness can affect mental health. Anxiety, depression, or fear of the future are common.
- Support groups and counseling can help.
- Sharing stories with others living with PBC reduces feelings of isolation.
Results and Call to Action
The treatment of primary biliary cirrhosis has come a long way. With modern medications, careful monitoring, and supportive care, most patients can live long, meaningful lives. As a doctor, I always remind my patients that early diagnosis and consistent care are the keys.
Now I’d love to hear from you:
- Are you or a loved one living with PBC?
- What treatment challenges or questions do you face?
Leave your questions in the comments, or book a consultation if you’d like professional guidance tailored to your situation.
Reference:
FAQS
Yes, although rare (about 10% of cases). Men with PBC may have slightly different disease patterns and need the same treatment approach.
Currently, there is no absolute cure, but effective treatments like UDCA and OCA slow progression and improve survival. In advanced cases, liver transplant can be life-saving.
Not necessarily. With early detection and treatment, many patients remain stable for years without major progression. Regular monitoring is key.
A liver-friendly diet includes fresh vegetables, lean proteins, whole grains, and plenty of fluids. Avoid alcohol, limit processed foods, and get adequate calcium and vitamin D.
With consistent treatment and lifestyle care, most patients have a good quality of life and long survival. Advanced therapies and research continue to improve outcomes.
🧑⚕️ About the Author
Dr. Asif, MBBS, MHPE
Dr. Asif is a licensed medical doctor and qualified medical educationist with a Master’s in Health Professions Education (MHPE) and 18 years of clinical experience. He specializes in gut health and mental wellness. Through his blogs, Dr. Asif shares evidence-based insights to empower readers with practical, trustworthy health information for a better, healthier life.
⚠️ Medical Disclaimer
This blog is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard or delay medical advice based on content you read here.

Leave a Reply