Hepatic Encephalopathy Caused by Cirrhosis – Introduction
Hepatic encephalopathy caused by cirrhosis is one of the complications that patients and families face while living with liver disease. As a physician and medical educator, I know how frightening this condition can seem but with early recognition and appropriate treatment, there is hope for improvement and recovery.
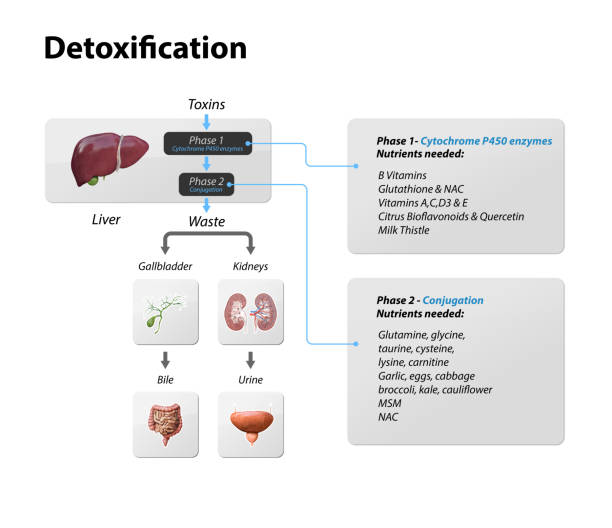
This article is written to simplify the complex medical science behind this condition. Imagine your liver as a filter that cleans toxins from your bloodstream, much like a water purifier. When cirrhosis (scarring of the liver) weakens that filter, toxins escape into the blood and reach the brain. This is what leads to hepatic encephalopathy (HE). Patients may experience confusion, memory problems, or even coma.
In this blog, I will explain what it means, why it happens, how it can be managed, and what modern medicine is doing to improve outcomes.
Hepatic Encephalopathy Caused by Cirrhosis – What Does It Really Mean
Hepatic encephalopathy caused by cirrhosis is a disorder where brain function is impaired because the liver cannot properly clear toxins such as ammonia. These toxins build up in the bloodstream and affect thinking, mood, sleep, and alertness. Patients may show confusion, irritability, forgetfulness, tremors, or even coma. It affects about 30-40% of cirrhotic patients. Prompt diagnosis and treatment can reverse symptoms, but relapses are common unless cirrhosis is resolved.
Understanding Hepatic Encephalopathy Caused by Cirrhosis
When patients ask me, “Dr., why does liver disease affect the brain?” Let me explain with a guess:
Think of your liver as your body’s chemical factory and waste disposal system. It processes nutrients, makes proteins, and detoxifies harmful substances. In cirrhosis, the factory walls become scarred and weakened. The waste (toxins like ammonia) is no longer cleaned up effectively. That waste then spreads into the bloodstream, travels to the brain, and disrupts its function.
Key facts:
- Found in 30-40% of cirrhotic patients (PubMed, 2022).
- Symptoms can range from mild forgetfulness to life-threatening coma.
- Early treatment can often reverse the condition.
Causes of hepatic encephalopathy in cirrhosis
Ammonia accumulation
The main culprit is ammonia, a byproduct of protein digestion. Normally, the liver detoxifies it into urea. In cirrhosis, ammonia builds up and affects the brain.
Precipitating factors
Even patients with stable cirrhosis can develop sudden encephalopathy if triggered by:
- GI bleeding (blood proteins increase ammonia load)
- Infection (such as pneumonia or UTI)
- Constipation (reduces ammonia clearance)
- Dehydration or electrolyte imbalance
- Medications (e.g., sedatives, painkillers)
For example, one of my patients with well-controlled cirrhosis suddenly developed confusion after severe constipation. Once treated, his alertness returned within two days.
Read [Cirrhosis Self-Care] to know in detail about precipitating factors of Cirrhosis and how to avoid it.
Symptoms of hepatic encephalopathy caused by cirrhosis.
Early symptoms hepatic encephalopathy (minimal HE)
- Mild forgetfulness
- Poor concentration
- Changes in sleep (daytime sleepiness, nighttime insomnia)
Progressive symptoms of hepatic encephalopathy
- Confusion or disorientation.
- Slurred speech
- Hand tremors (Asterixis, or “liver flap”)
- Changes in mood or personality
Severe symptoms of hepatic encephalopathy
- Extreme drowsiness
- Inability to perform daily tasks.
- Coma (medical emergency)
Stages of Hepatic Encephalopathy
Doctors classify HE into grades (I-IV):
- Grade I: Mild changes in attention, irritability, sleep disturbances.
- Grade II: Disorientation, lethargy, personality changes.
- Grade III: Severe confusion, unusual behavior, inability to function.
- Grade IV: Coma.
This helps guide the urgency of treatment and the diagnosis.
Diagnosis of hepatic encephalopathy in cirrhosis
The diagnosis is clinical but is supported by tests.
Physical examination
- History of cirrhosis
- Neurological examination (memory, alertness, tremor testing)
Lab tests
- Blood ammonia levels (may not always correlate with severity)
- Liver function tests
- Kidney function and electrolytes
Imaging and other tests
- CT/MRI to rule out stroke or bleeding
- EEG (electrical activity of the brain) in unclear cases
Reference: Mayo Clinic – Hepatic encephalopathy
Treatment of hepatic encephalopathy due to cirrhosis
Treatment of hepatic encephalopathy due to cirrhosis focuses on two goals:
- Controlling immediate symptoms by reducing the accumulation of toxins in the blood.
- Preventing recurrence by addressing the underlying triggers and managing the cirrhosis itself.
Here are the main strategies:
Correcting precipitating factors
Often, hepatic encephalopathy is triggered by another medical problem. Unless the trigger is corrected, treatment will not be successful. Common triggers and their management include:
- Gastrointestinal bleeding → Treated with endoscopy, medications, or blood transfusions.
- Infections (UTIs, pneumonia, peritonitis) → Antibiotics and supportive care.
- Constipation → Laxatives or stool softeners.
- Dehydration and electrolyte imbalance → Correct IV fluids, sodium/potassium levels.
- Sedatives or narcotics → Reduce or stop the offending medication.
Example: I once treated a patient who became severely confused after taking sleeping pills. Once we stopped the medication and gave him lactulose, he improved within 48 hours.
Medications to Reduce Ammonia
Lactulose (First-Line Therapy)
- A nondigestible sugar that traps ammonia in the intestine and helps remove it through stool.
- Goal: 2-3 soft bowel movements per day.
- Give orally or by enema if the patient cannot swallow.
Patients and families are sometimes concerned when I tell them that we need more than one soft stool per day but it is an important part of treatment.
Rifaximin (Add-on Therapy)
- A non absorbable antibiotic that reduces ammonia-producing gut bacteria.
- Often combined with lactulose, especially in recurrent cases.
- Studies show that it reduces the risk of recurrence and improves quality of life.
Other drugs under study
- L-ornithine L-aspartate (LOLA): Promotes breakdown of ammonia in the liver and muscles.
- Probiotics: Improve gut microbiome balance, showing some benefit in mild HE.
- Zinc supplements: May help in selected patients, as zinc is a cofactor for ammonia detoxification.
Supportive care
- IV fluids and electrolytes to maintain hydration and balance.
- Nutritional support: Balanced protein diet, emphasizing plant proteins and dairy rather than red meat alone.
- Hospitalization for moderate to severe cases.
Liver transplant
For patients with advanced cirrhosis, liver transplant is the only definitive treatment. After transplant, hepatic encephalopathy usually disappears as the new liver effectively clears toxins.

Promising advances in treatment and recovery
While standard treatments such as lactulose and rifaximin remain essential, research in recent years has made promising advances in the treatment and rehabilitation of patients with hepatic encephalopathy due to cirrhosis.
Microbiome-targeted therapies
Scientists are learning that the gut microbiome plays a major role in ammonia production. Promising advances include:
- Probiotics and synbiotics (probiotics + prebiotics): Early trials show they reduce HE recurrence.
- Fecal microbiota transplantation (FMT): Still experimental, but some studies suggest it improves cognition in recurrent HE.
New drug developments
- Glycerol phenylbutyrate (GPB): Helps remove nitrogen from alternative pathways.
- Ornithine phenylacetate (OP): Experimental drug that reduces ammonia levels in the blood.
- Novel antibiotics: Target specific bacteria without disrupting the entire microbiome.
Digital and early detection tools
- Smartphone based cognitive tests can detect early HE before family members notice changes.
- Driving simulators and reaction time apps can prevent accidents in early HE patients.
Rarely discussed insight: In my experience, patients often notice “subtle errors” before they notice family confusion at work or while driving. These small changes are early warning signs that new tools can now catch.
Personalized nutrition and exercise
- Prepared protein plans: Instead of restricting protein (the old practice), current guidelines encourage a balanced diet with more plant protein.
- Branched-chain amino acid (BCAA) supplements: May improve muscle ammonia metabolism.
- Exercise: Even light activity increases muscle mass, which helps detoxify ammonia outside the liver.
Improved liver transplant outcomes
Advances in surgical techniques and post transplant care have improved survival rates. Many patients who once faced repeated hospitalizations for HE are now enjoying long, healthy lives after transplantation.
Reference: WHO – Liver cirrhosis and complications
Prognosis and long-term outlook
- 1-year survival after first HE episode: ~60% (PubMed, 2021).
- Recurrence without continued treatment is common.
- Liver transplant offers the best long-term survival.
Read in Detail: Liver life expectancy stage 4 cirrhosis
Prevention of hepatic encephalopathy due to cirrhosis
Lifestyle measures
- Low protein diets are outdated; instead, balanced protein with more plant sources is recommended.
- Avoid constipation.
- Take medications exactly as prescribed.
Prevent the progression of cirrhosis.
- Manage hepatitis B and C.
- Avoid alcohol.
- Maintain a healthy weight.
Read in Detail About: How to keep your liver healthy.
Conclusion and call to action.
Hepatic encephalopathy due to cirrhosis is a serious but manageable condition. With timely treatment, lifestyle adjustments, and medical follow up, many patients regain clarity and improve their quality of life.
As a doctor, I have seen families feel deep relief when a loved one “comes back” after treatment. Awareness and early action make all the difference.
Have you or a loved one experienced hepatic encephalopathy? Share your questions or experiences in the comments below. If you have concerns, don’t wait consult your doctor or refer to a liver specialist.
FAQS
Yes. With prompt treatment, symptoms can improve or fully resolve, especially in early stages. However, recurrence is common unless the underlying cirrhosis is managed.
No. Around 30–40% of cirrhotic patients develop HE, but good self-care and treatment can reduce risk.
It varies. Some patients worsen within hours after a trigger (like GI bleeding), while others have gradual decline over weeks.
No. Unlike dementia, HE can be reversible with treatment. However, repeated episodes may cause long-term memory issues.
🧑⚕️ About the Author
Dr. Asif, MBBS, MHPE
Dr. Asif is a licensed medical doctor and qualified medical educationist with a Master’s in Health Professions Education (MHPE) and 18 years of clinical experience. He specializes in gut health and mental wellness. Through his blogs, Dr. Asif shares evidence-based insights to empower readers with practical, trustworthy health information for a better, healthier life.
⚠️ Medical Disclaimer
This blog is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard or delay medical advice based on content you read here.

Leave a Reply