Introduction
Can hepatitis cause cirrhosis? This is one of the most common and important questions patients ask me in the clinic. Hepatitis, which simply means inflammation of the liver, can range from mild and temporary to severe and life threatening. When left untreated or left to progress, chronic hepatitis can actually damage the liver so much that it leads to cirrhosis a condition where normal liver tissue is replaced with scar tissue, reducing its ability to function.
As a physician and medical educator, I have seen many patients confused about whether hepatitis always leads to cirrhosis or whether it can be prevented. In this guide, I will explain the link step-by-step using clear examples, real research, and practical insights that are easy to understand even without a medical background.
Can hepatitis cause cirrhosis?
Yes, hepatitis especially chronic forms like hepatitis B and C can cause cirrhosis if left untreated. This process usually takes 10 to 30 years, depending on the type of virus, lifestyle, and the presence of other health risks (such as alcohol use or obesity). Hepatitis leads to persistent inflammation of the liver. Over time, the liver responds by forming scar tissue. This scar gradually replaces healthy liver tissue, leading to cirrhosis. Not everyone with hepatitis develop cirrhosis, but chronic hepatitis is one of the leading causes of cirrhosis and liver failure worldwide. Early diagnosis, antiviral treatment, vaccination (for hepatitis B), and lifestyle changes can significantly reduce the risk.
What is hepatitis?
Hepatitis means inflammation of the liver. Think of the liver as a water filter: It removes toxins, processes nutrients, and balances the body’s chemistry. If the filter becomes clogged or damaged repeatedly, it stops working properly. This is exactly what happens when hepatitis persists.
Types of Hepatitis
- Hepatitis A – Short-term, spread through contaminated food/water. Rarely leads to cirrhosis.
- Hepatitis B – Can become chronic; major risk factor for cirrhosis and liver cancer.
- Hepatitis C – Most likely to become chronic and progress to cirrhosis silently.
- Hepatitis D – Occurs only with hepatitis B infection, increases risk of cirrhosis.
- Hepatitis E – Similar to A, mostly acute but can be severe in pregnancy.
For more details, see our blog [Hepatitis C Viral Infection] and [Hepatitis B Causes]
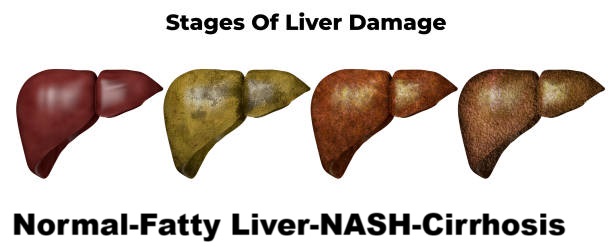
What is cirrhosis?
Cirrhosis is like a city slowly being taken over by cement. Instead of flexible, functioning tissue, scar tissue (fibrosis) spreads throughout the liver. Once cirrhosis develops, the liver struggles to filter toxins, make proteins, or regulate digestion.
Stages of cirrhosis
- Compensated cirrhosis – early stage; liver still functions, symptoms are mild or absent.
- Decompensated cirrhosis – severe damage; complications such as ascites (fluid in the abdomen), variceal bleeding, jaundice, and encephalopathy develop.
For patient care, check out Cirrhosis Self-Care

Hepatitis can cause cirrhosis? Step by step progression
Yes, hepatitis can cause cirrhosis, but it doesn’t happen overnight. The process takes years.
Stage 1 – Chronic inflammation
When hepatitis viruses (especially B and C) remain in the body, they continually inflame the liver. Imagine scratching the same spot on your skin every day. It won’t heal properly and will scar.
Stage 2 – Fibrosis develops
The liver tries to heal, but repeated injury causes fibrosis (scarring). Initially, the scarring is patchy.
Stage 3 – Advanced fibrosis
Fibrosis spreads throughout the liver tissue, restricting blood flow and the exchange of nutrients.
Stage 4 – Cirrhosis
When most of the liver is scarred, cirrhosis develops. Complications appear at this stage.
According to WHO, approximately 20-30% of chronic hepatitis B patients and 15-30% of chronic hepatitis C patients develop cirrhosis within 20 years. WHO Hepatitis Fact Sheet
Risk factors that accelerate cirrhosis in hepatitis patients.
Not every patient with hepatitis develop cirrhosis. Certain factors increase the risk:
- Alcohol consumption (loss of synergy with hepatitis C).
- Obesity and fatty liver disease.
- Diabetes and insulin resistance.
- HIV co-infection.
- Male gender and older age.
- Genetic predisposition.
Symptoms of cirrhosis from hepatitis
Cirrhosis can be silent for years, which is why regular check ups are so important.
Early Symptoms
- Fatigue
- Mild Abdominal Pain
- Loss of Appetite
Advanced Symptoms
- Jaundice (yellow skin/eyes)
- Swelling in the legs and abdomen
- Confusion (hepatic encephalopathy)
- Vomiting blood (vesicular blood)
Read: [First Sign of Hepatitis C] and [Early Symptoms of Hepatitis B] For early warning signs.
Do Hepatitis B and C Cause Cirrhosis Differently?
Yes, although both hepatitis can cause cirrhosis, the pathways and risks are different.
- Hepatitis B: The immune system’s response damages the liver. Some patients clear it, others carry it for life.
- Hepatitis C: Slowly progressive but more consistently chronic.
CDC data shows that 25% of adults with chronic hepatitis B and up to 20% of people with hepatitis C will develop cirrhosis within 20 years. CDC Hepatitis Statistics
Read: Can Hepatitis C Cause Cirrhosis. For an in depth explanation.
Doctor Insights – What I See in the Clinic.
As a physician, I often see patients who never knew they had hepatitis until cirrhosis had already progressed. One patient, a 42 year old man, had mild fatigue and bloating. He ignored it until one day he developed jaundice. Tests revealed hepatitis C along with cirrhosis.
This highlights why early screening and treatment are life saving. Most people assume that cirrhosis is only related to alcohol, but viral hepatitis is just as dangerous often more silent.
Prevention of cirrhosis in hepatitis.
Prevention of cirrhosis in hepatitis patients is possible with proper medical care and lifestyle changes. Although not every case of hepatitis develop cirrhosis, early action can dramatically reduce your risk.
Get vaccinated (hepatitis A and B)
- If you are not already infected with hepatitis B, vaccination provides strong protection.
- The hepatitis A vaccine is also recommended to prevent additional stress on the liver.
- Vaccination reduces your overall risk of complications.
Take recommended antiviral treatment.
- Hepatitis B: Antiviral drugs (such as tenofovir, entecavir) can suppress the virus and reduce liver damage.
- Hepatitis C: Direct acting antivirals (DAAs) can cure the infection in 95% of cases.
Skipping or delaying treatment increases the risk of scarring.
The Mayo Clinic notes that DAAs for hepatitis C can reduce the risk of cirrhosis by more than 70 percent.
Avoid alcohol completely.
- Alcohol is like “fuel on a fire” for a liver damaged by hepatitis.
- Even small amounts accelerate the progression of fibrosis.
- Hepatitis patients should completely quit drinking alcohol, not just cut down.

Maintain a healthy weight and diet
- Obesity and fatty liver worsen hepatitis related scarring.
Focus on:
- High-fiber foods (whole grains, vegetables, legumes)
- Lean proteins (chicken, fish, beans)
- Low in sugar and processed foods
- Avoid excessive red meat and fried foods.
Manage other health conditions.
- Diabetes, high cholesterol, and high blood pressure increase your risk of cirrhosis.
- Regular checkups and medications keep them under control.
- Talk to your doctor about how to balance medications that affect the liver.
Regular monitoring and checkups
- Ultrasound scans and FibroScan help detect early fibrosis.
- Blood tests (ALT, AST, bilirubin) show liver health.
- Hepatitis patients should ideally have checkups every 6-12 months.
Avoid unnecessary medications and toxins.
- Overuse of painkillers (such as acetaminophen) can damage the liver.
- Herbal supplements are not always safe and may worsen the damage.
- Always consult your doctor before taking new medications.
Strengthen your immune system
- Proper sleep, stress management, and a balanced diet help support immunity.
- A strong immune response can better control viral activity.
Stop smoking
- Smoking increases oxidative stress on the liver.
- Combined with hepatitis, it worsens long term outcomes.
Treat complications early
- See a doctor immediately if symptoms such as swelling, jaundice, or fatigue appear.
- Early intervention prevents cirrhosis from getting worse quickly.
Conclusion and Call to Action
So, can hepatitis cause cirrhosis? The answer is yes especially with chronic hepatitis B and C. But cirrhosis doesn’t happen overnight, and with vaccinations, treatment, and healthy lifestyle choices, the risk can be significantly reduced.
As a doctor, I strongly encourage you: If you have hepatitis, don’t wait. Get tested, start treatment early, and take steps to protect your liver.
Your turn: Have you or a loved one dealt with hepatitis or cirrhosis? Share your story in the comments, or ask me your questions. Together, we can spread awareness and prevent liver disease.
References:
FAQS
Early fibrosis may improve with treatment, but established cirrhosis is usually permanent. However, progression can be slowed or halted.
No. Not every patient with hepatitis develops cirrhosis. It depends on whether the infection becomes chronic, how strong the immune response is, and risk factors like alcohol use or obesity.
Follow medical advice strictly: take antivirals, avoid alcohol, eat liver-friendly foods, maintain a healthy weight, and attend regular check-ups.
Typically, 10–30 years. Some patients progress faster if multiple risk factors are present, while others never reach cirrhosis if treated early.
Hepatitis B and C are the leading causes worldwide. Hepatitis C is more likely to become chronic, while hepatitis B carries an additional risk of liver cancer.
🧑⚕️ About the Author
Dr. Asif, MBBS, MHPE
Dr. Asif is a licensed medical doctor and qualified medical educationist with a Master’s in Health Professions Education (MHPE) and 18 years of clinical experience. He specializes in gut health and mental wellness. Through his blogs, Dr. Asif shares evidence-based insights to empower readers with practical, trustworthy health information for a better, healthier life.
⚠️ Medical Disclaimer
This blog is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard or delay medical advice based on content you read here.

Leave a Reply