Introduction
Fatty Liver Grades A Key Insight into Liver Health
As a practicing physician and medical educator, I often meet patients who are surprised when they are told they have “fatty liver.” One of the first questions they ask is “How bad is it?” That’s where fatty liver grades come in.
Understanding fatty liver grades is important because it helps you and your healthcare provider assess how advanced your condition is and whether you can reverse it with simple lifestyle changes or if you are already at risk for more serious liver damage.
In this guide, I will tell you about the grading system, how each grade is diagnosed, and what you can do to manage and even reverse the damage. I will also share a real patient’s experience and some clinical insights to answer a very common query that can fatty liver be reversed?
What is fatty liver? (A quick summary before diving into the grades)
Fatty liver, or hepatic steatosis, occurs when fat builds up in liver cells. It’s often caused by a poor diet, lack of exercise, obesity, insulin resistance, and alcohol use. There are two main types:
- Non-alcoholic fatty liver disease (NAFLD)
- Alcoholic fatty liver disease (AFLD)
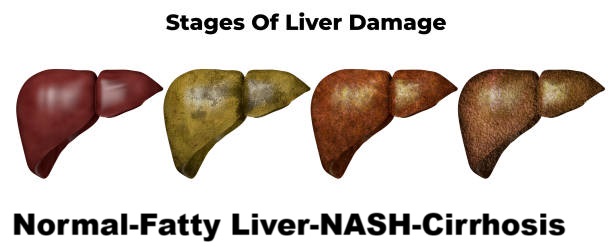
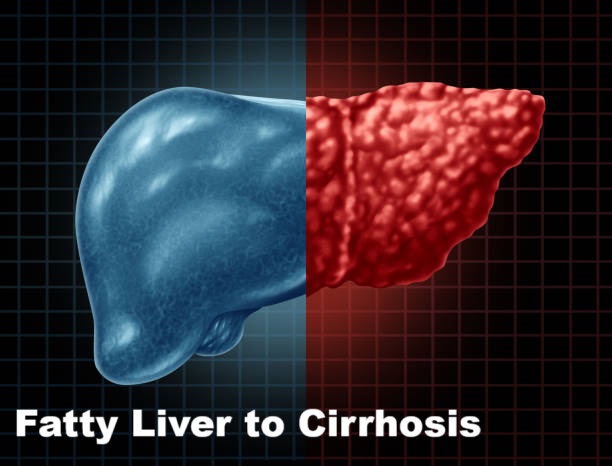
Over time, fatty liver can progress to non-alcoholic steatohepatitis (NASH), fibrosis, and eventually cirrhosis, which is irreversible liver scarring.
[Fatty liver disease explained Read a Complete Article]
Fatty liver grades: What they mean.
The fatty liver grading system grades the severity of fat accumulation in the liver. It is usually diagnosed by ultrasound, CT scan, or MRI, and is sometimes confirmed by a liver biopsy or fibroscan.
There are three main grades of fatty liver:
Grade 1 fatty liver (mild steatosis)
Fatty infiltration: Less than 33% of liver cells contain fat.
Symptoms: Often asymptomatic; may feel a little tired or have a slight heaviness in the abdomen.
Liver function: Usually normal.
What you should know:
This is the most reversible stage. With diet and exercise, many patients completely normalize their liver enzymes within 3-6 months.
[Read Liver cleansing diet plan]
Grade 2 Fatty Liver (Moderate Steatosis)
Fatty infiltration: 33-66% of liver cells are affected.
Symptoms: Fatigue, bloating, mild right upper quadrant discomfort.
Liver function: May begin to show mild abnormalities in ALT and AST.
Clinical insight:
At this point, inflammation can begin, increasing the risk of progression to NASH if left unchecked.
“Many patients with Grade 2 fatty liver I have seen have metabolic syndrome diabetes, high blood pressure, and obesity. Addressing these together is key to reversing liver damage.”
Grade 3 Fatty Liver (Severe Steatosis)
Fatty infiltration: More than 66% of liver cells are loaded with fat.
Symptoms: More pronounced fatigue, bloating, and even mild jaundice in rare cases.
Liver function: Often abnormal. Fibrosis (early scarring) may already be present.
Why it’s serious:
This stage is often a precursor to NASH and cirrhosis. According to a 2020 study published in PubMed (PMID: 32083839), up to 25% of patients with grade 3 fatty liver may progress to cirrhosis over time.
[Difference Between Fatty Liver and Cirrhosis Read it Here]
How are fatty liver grades diagnosed?
1. Ultrasound (USG)
The most common and non-invasive method. Radiologists evaluate the brightness, echogenicity, and visibility of the vessels to assign a grade.
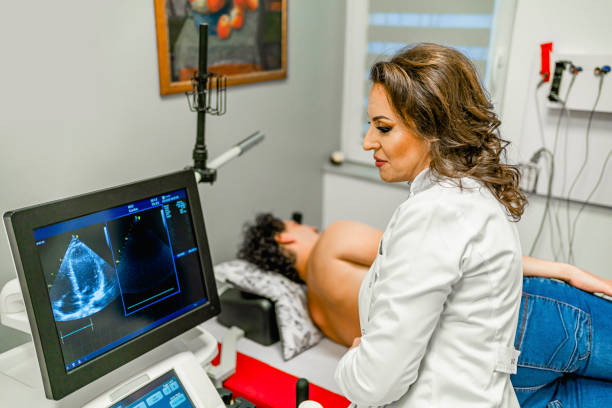
2. FibroScan or transient Elastography
Measures the stiffness and fat content of the liver.
3. MRI or CT scan
More accurate but expensive. MRI-PDFF can quantify the percentage of fat in liver tissue.
4. Liver function tests
Look at ALT, AST, GGT levels but remember, you can have grade 2 or 3 fatty liver with normal labs.
5. Liver biopsy
The gold standard but rarely needed unless NASH or advanced fibrosis is suspected.
Risk factors that affect fatty liver grades
Several lifestyle and genetic factors contribute to worsening fatty liver disease:
- Obesity – especially central obesity
- High intake of sugar or processed foods
- Diabetes or insulin resistance
- Sedentary lifestyle
- Alcohol consumption (even in small amounts)
- Polycystic ovary syndrome (PCOS) in women
- Lack of sleep and chronic stress
Can fatty liver be reversed?
Can fatty liver be reversed is a question every fatty liver patient is concerned and the answer is:
Yes, especially grade 1 and grade 2 fatty liver can be reversed. Grade 3 requires more aggressive management and close monitoring.
- Lifestyle changes that work:
- Lose 7-10% of body weight.
- Exercise at least 150 minutes per week (brisk walking, strength training)
- Adopt a liver-friendly diet
- High fiber (vegetables, whole grains)
- Healthy fats (olive oil, avocado)
- Avoid sugary drinks, red meat, refined carbohydrates.
[Liver Cleansing Diet Plan will help you to reverse fatty liver]

Real case example: From Grade 2 to Grade 0 in 6 months
A 37-year-old IT professional came in for a routine health checkup and was diagnosed with Grade 2 fatty liver on ultrasound. He had a BMI of 30, high triglycerides, and borderline sugar. Along with:
- Customized diet plan
- Intermittent fasting
- 45-minute daily walk
6 months later his repeat ultrasound showed no fat in the liver. ALT and AST returned to normal, and he lost 8 kg.
Rarely Discussed Insight: Genetics and Ethnicity Matter
In clinical practice, I have observed that South Asian and Middle Eastern populations often develop fatty liver at a lower BMI than Western populations.
In addition, certain gene variants, such as PNPLA3 and TM6SF2, put some individuals at higher risk of fat accumulation despite a relatively healthy lifestyle.
This is why screening and early lifestyle interventions are important even in people who “appear healthy.”
Complications of ignoring fatty liver Grades
If left untreated, fatty liver can lead to:
- NASH (non-alcoholic steatohepatitis)
- Fibrosis (early scarring)
- Cirrhosis (irreversible scarring)
- Liver cancer (hepatocellular carcinoma)
According to the WHO, NAFLD is now the leading cause of chronic liver disease globally, affecting more than 25% of the world’s population (WHO NAFLD data).
When to see a doctor
If you have been told you have fatty liver or have symptoms such as:
- Unexplained fatigue
- Pain in the right upper abdomen
- Elevated liver enzymes
- Family history of liver disease
Make an appointment with your doctor. Early diagnosis and staging can completely change the outcome.
Trusted sources for further reading
CDC – Nonalcoholic fatty liver disease (NAFLD)
Mayo Clinic – Fatty liver disease
Final thoughts: Fatty liver levels are a wake-up call, not a life sentence
Fatty liver levels aren’t just numbers on a report card they reflect the health of your liver.
The good news? You can reverse most fatty liver levels, especially if caught early. But you need to take action now.
Call to action
- Have you or someone you know been diagnosed with fatty liver?
- Leave your questions in the comments, and I’ll be happy to answer them.
- Or better yet book a consultation to get a personalized liver health plan.
Your liver is silent, but don’t wait for it to scream. Take care of it today.
FAQS
Yes, in its early stages (especially Grade 1), fatty liver is often reversible with lifestyle changes. The goal is to address the underlying causes to prevent the disease from progressing.
- Grade 1: Highly reversible. The focus is on weight loss (even 3-5% of body weight can make a difference), a healthy diet, and regular exercise.
- Grade 2: Reversible, but it requires more significant and consistent effort. Lifestyle changes are crucial, and sometimes medications to manage related conditions like diabetes or high cholesterol may be prescribed.
- Grade 3: While the scarring (fibrosis) in this stage may not be fully reversible, it is still possible to halt the progression of the disease and prevent it from advancing to cirrhosis. Treatment focuses on a combination of lifestyle changes and medical management of complications.
Currently, there is no single approved drug to cure or reverse fatty liver disease itself. However, medications may be used to treat the associated conditions that contribute to fatty liver, such as diabetes and high cholesterol. New drugs are being researched and some have recently been approved for specific types of fatty liver disease.
One of the most challenging aspects of fatty liver disease is that it often presents with no symptoms, especially in its early stages (Grade 1). When symptoms do appear, they are often non-specific and can include:
- Grade 1: Usually asymptomatic. Some people may experience mild fatigue or a dull ache in the upper right abdomen.
- Grade 2: Symptoms may become more noticeable and can include persistent fatigue, general malaise, or a feeling of discomfort in the upper right abdomen.
- Grade 3: Symptoms are more severe and can be a sign of advanced liver damage. These may include fatigue, unexplained weight loss, abdominal swelling (ascites), jaundice (yellowing of the skin and eyes), and easy bruising
The primary causes are often related to lifestyle and metabolic conditions:
- Unhealthy Diet: Diets high in refined sugars, saturated fats, and processed foods are major contributors.
- Obesity and Overweight: Excess body weight, particularly around the abdomen, is a significant risk factor.
- Insulin Resistance and Diabetes: These conditions can disrupt the body’s fat metabolism, leading to fat accumulation in the liver.
- High Cholesterol and Triglycerides: Abnormal lipid levels in the blood are closely linked to fatty liver.
- Excessive Alcohol Consumption: This is a leading cause of a specific type of fatty liver disease (alcoholic fatty liver disease)
🧑⚕️ About the Author
Dr. Asif, MBBS, MHPE
Dr. Asif is a licensed medical doctor and qualified medical educationist with a Master’s in Health Professions Education (MHPE) and 18 years of clinical experience. He specializes in gut health and mental wellness. Through his blogs, Dr. Asif shares evidence-based insights to empower readers with practical, trustworthy health information for a better, healthier life.
⚠️ Medical Disclaimer
This blog is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard or delay medical advice based on content you read here.


Leave a Reply